Patient privacy is more than a legal requirement it’s a core element of trust between patients and healthcare providers. In the medical billing process, sensitive information moves through multiple systems, platforms, and personnel. Each step presents potential risks if privacy isn’t protected with the right policies and technology.
In this guide, we explain why patient privacy matters in medical billing, how it affects patients, physicians, and healthcare business owners, and what best practices every organization should follow.
What Is Patient Privacy in Medical Billing?
Patient privacy refers to safeguarding Protected Health Information (PHI) during the documentation, coding, billing, and claims submission process.
Key entities involved include:
- Patients – the data owners
- Healthcare providers – clinics, hospitals, physicians
- Medical billing companies – internal or outsourced
- Insurance payers – Medicare, Medicaid, commercial insurers
- Health Information Systems – EHR, PMS, clearinghouses
- Regulatory bodies – HIPAA, HITECH, OCR
PHI includes attributes such as:
- Patient name, address, phone number
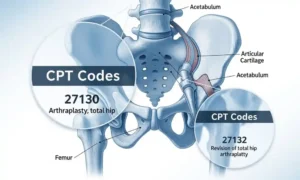
- Medical history, diagnosis codes
- Procedure codes
- Insurance policy details
- Billing statements
- Social Security numbers and demographic data
Protecting these attributes at every touchpoint is essential to preventing data breaches, fraud, and compliance penalties.
Why Patient Privacy Matters: Key Reasons
1. It Protects Patients from Identity Theft and Fraud
Medical identity theft is one of the fastest-growing cybercrimes. Stolen PHI can be used to:
- File false insurance claims
- Obtain medical services illegally
- Create fake identities
A single exposed billing statement may contain enough data for criminals to cause long-term financial and medical harm.
2. It Builds Trust Between Patients and Providers
Patients expect their personal and medical details to stay confidential.
When billing processes are secure, it enhances:
- Patient satisfaction
- Brand reputation
- Long-term loyalty
- Transparency in healthcare services
Trust directly impacts a provider’s ability to retain and engage patients.
3. It Ensures Compliance With HIPAA and Other Regulations
Healthcare organizations must comply with:
- HIPAA Privacy Rule
- HIPAA Security Rule
- HITECH Act
- State-specific privacy laws
Failing to protect billing-related PHI may result in:
- Heavy civil penalties
- Litigation
- Loss of licensure
- Damage to reputation
Compliance isn’t optional—it’s a legal requirement.
4. It Improves Operational Efficiency
Privacy-driven processes often produce clearer workflows:
- Accurate coding
- Error-free claims submission
- Fewer rejected or denied claims
- Faster reimbursement cycles
Secure and well-documented billing systems lead to smoother revenue operations.
5. It Reduces Risk of Data Breaches
Breaches can occur through:
- Unsecured email
- Weak passwords
- Misplaced paper statements
- Outdated billing software
- Human error
A strong privacy framework reduces the likelihood of breaches and protects the organization from financial loss.
Who Benefits From Strong Patient Privacy Practices?
Patients
- Protection from misuse of PHI
- Peace of mind
- Controlled sharing of medical data
- Trust in healthcare services
Doctors & Healthcare Providers
- Reduced legal and compliance risks
- More efficient billing cycles
- Better patient relationships
- Higher patient retention
Medical Billing Companies & Business Owners
- Enhanced credibility
- Fewer claim rejections
- Stronger partnerships with providers
- Scalable and secure operations
Privacy is not just ethical—it is an essential component of business success.
Common Questions Patients Ask About Billing Privacy
1. Who has access to my billing information?
Only authorized personnel such as billing staff, coders, insurance payers, and providers directly involved in your care.
2. Are my medical bills shared with third parties?
Only as required for insurance, claims processing, or legal compliance. Providers must have Business Associate Agreements (BAAs) in place.
3. How is my information stored?
Most healthcare organizations use encrypted EHR/PMS systems with restricted access and audit trails.
4. What should I do if I suspect my medical data was leaked?
Contact your provider, request an accounting of disclosures, and consider placing a fraud alert with credit agencies.
Best Practices for Protecting Patient Privacy in Medical Billing
For Healthcare Providers & Billing Companies
- Encrypt all PHI during storage and transmission
- Use secure patient portals instead of email
- Limit access using role-based permissions
- Conduct regular HIPAA training for all staff
- Implement multi-factor authentication (MFA)
- Maintain updated billing and EHR software
- Use secure shredding practices for paper documents
- Complete routine system audits and risk assessments
For Patients
- Ask how your data is stored and used
- Use secure portals for billing communication
- Review statements for unusual transactions
- Report suspected fraud immediately
The Role of Technology in Patient Privacy
Modern billing systems include tools that improve privacy and compliance:
- Electronic Health Records (EHR)
- Practice Management Systems (PMS)
- Encrypted digital billing platforms
- AI-driven auditing tools
- Secure clearinghouses
These systems automate protection through:
- Access logs
- Data encryption
- Automatic error detection
- Secure integrations
Technology is now a frontline defense in patient data protection.
Conclusion: Privacy Is the Foundation of Trust in the Billing Process
Patient privacy is more than compliance—it’s a commitment to patient dignity, safety, and trust.
For healthcare providers and business owners, protecting PHI ensures:
- Better patient relationships
- Improved financial performance
- Safer and more efficient billing operations
- Full regulatory compliance